
COMPLETE SOLUTION FOR MEDICARE & MEDICAID CERTIFICATION
Take the first step toward compliance and certification success
Complete Solution For Medicare & Medicaid Certification Guidance For Providers
At CarePolicy.US, we recognize that obtaining Medicare and Medicaid certification is one of the most important steps for agencies seeking to expand their services and serve federally funded clients. Navigating the CMS enrollment process, PECOS registration (PECOS registration means signing up and creating an account in the Provider Enrollment, Chain, and Ownership System (PECOS), which is the official online system used by CMS (Centers for Medicare & Medicaid Services)), and state Medicaid requirements can feel overwhelming for both new and established providers. That’s why we’ve developed a comprehensive Medicare & Medicaid Licensing Support Package, designed to guide agencies through every step of the certification journey with confidence and efficiency.
Our package covers the full scope of support needed to achieve certification, including CMS enrollment, PECOS application filing, policy and documentation alignment, survey preparation, and Medicaid provider enrollment. Whether you are a Home Health Agency, Assisted Living Facility, Personal Care Home, or Behavioral Health provider, our dedicated team ensures your agency is ready to meet federal and state compliance requirements without unnecessary delays.
With deep knowledge of the Conditions of Participation (CoPs), CMS standards, and state Medicaid program guidelines, our consultants provide tailored guidance to help your agency avoid common pitfalls and accelerate approval. From initial application to ongoing compliance, we partner with you to ensure your organization is positioned for long-term success in serving Medicare and Medicaid clients.
Why Our Certification Support?
-
Comprehensive CMS Enrollment Guidance
We guide agencies through the fullCenters for Medicare & Medicaid Services (CMS) enrollment process,including PECOS registration, provider enrollment forms, and state surveyreadiness. Our team ensures your application meets both state and federal compliancestandards.
-
Medicare & Medicaid Certification Preparation
Our consultants provide hands-on support to prepare your agency for Medicare and Medicaid certification surveys, including policy alignment, staff training, and mock audits. This preparation minimizes the risk of deficiencies and accelerates certification approval.
-
Documentation & Policy Alignment
Our experts review and customize yourpolicies, procedures, and compliance manuals to ensure alignment with CMSConditions of Participation and Medicaid requirements.
-
License Guaranteed
We provide a 100% compliance package with guaranteed approval, working with you through any state feedback until your agency is fully licensed and approved — provided your information is complete, accurate, and background checks are clear.
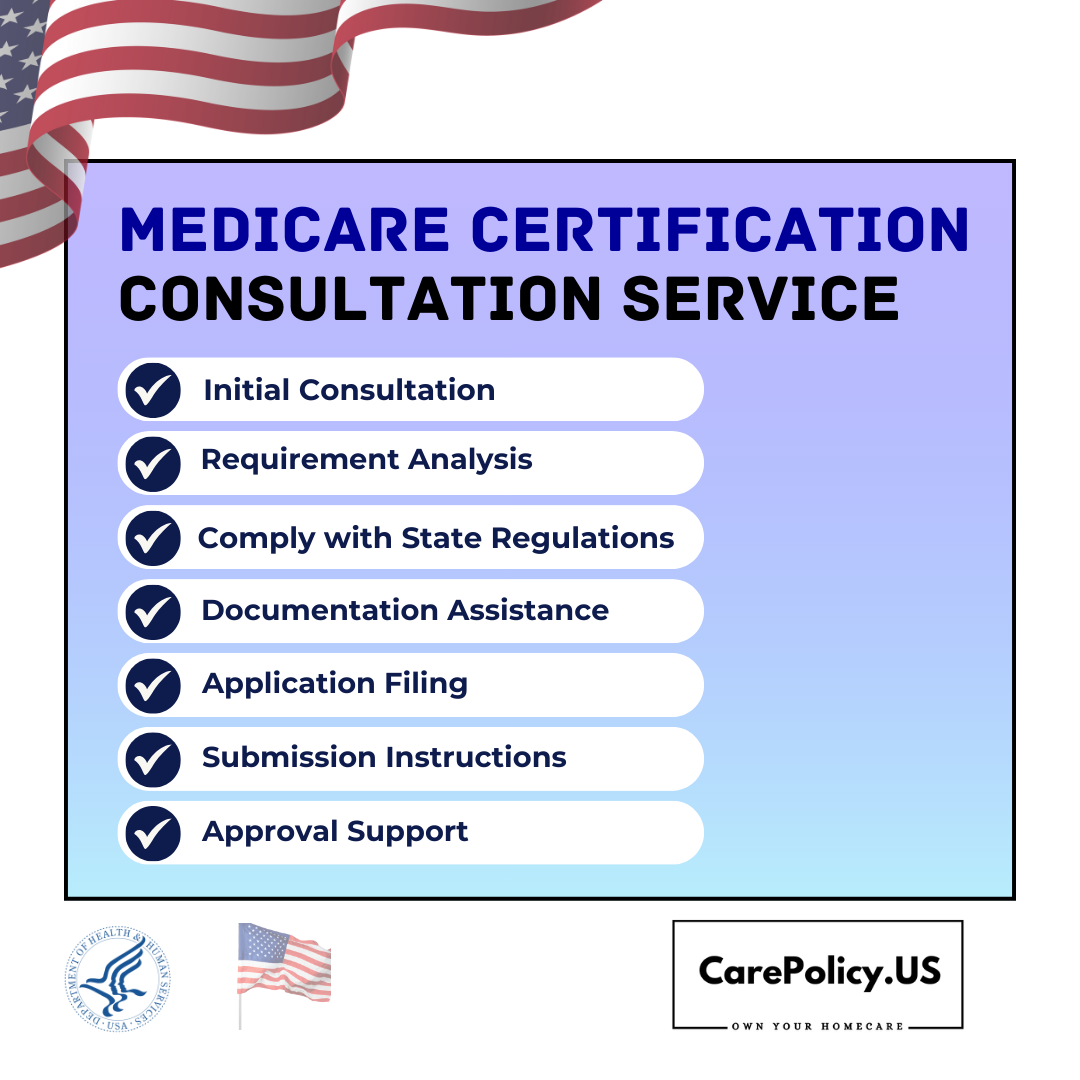
Medicare Certification Consultation Service
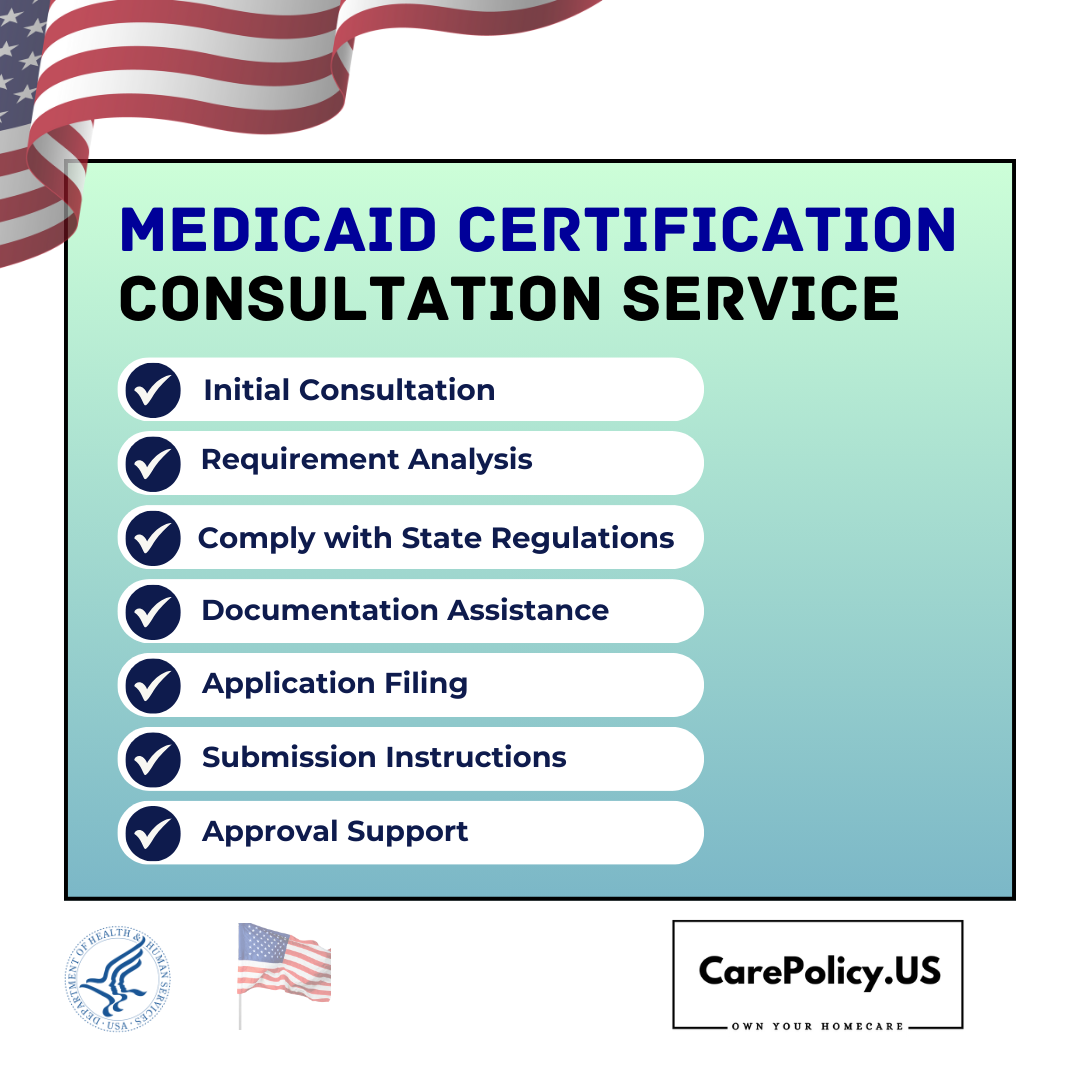
Medicaid Certification Consultation Service
Frequently Asked Questions (FAQ) for Medicare & Medicaid Certification Services
What is the difference between state licensure and Medicare/Medicaid certification?
State licensure allows your
agency to legally operate within your state, while Medicare and Medicaid
certification enables your agency to serve federal and state-funded clients and
receive reimbursements through CMS.
Do I need to be licensed before applying for Medicare/Medicaid certification?
Yes. State licensure is a
prerequisite. Once licensed, agencies can proceed with CMS enrollment and the
certification survey process.
Do I need separate applications for Medicare and Medicaid?
Yes. While both are government programs, Medicare enrollment is through CMS (via PECOS), and Medicaid enrollment is through your state program. We handle both processes and ensure your applications align.
How long does it take to become Medicare and/or Medicaid certified?
The process can take anywhere from 3 to 9 months, depending on state survey schedules, CMS processing times, and your agency’s readiness. Our preparation helps shorten delays and avoid resubmissions.
What documents are required for Medicare/Medicaid certification?
Required documents may include: NPI confirmation, ownership disclosure, organizational policies, clinical policies (if applicable), proof of state license, and financial documents. We provide a customized checklist for your agency.
Will you assist with PECOS and CMS enrollment?
Yes. We handle PECOS registration, CMS Form 855 enrollment, and survey readiness, ensuring accuracy to prevent delays.
What if my agency fails the initial CMS survey?
If deficiencies are cited, we help you prepare a Plan of Correction (POC) and guide you through resubmission until certification is achieved.
Can CarePolicy.US assist with Medicaid enrollment as well?
Absolutely. We support Medicaid provider enrollment for your state, ensuring compliance with Medicaid-specific requirements.
What if my agency doesn’t pass the first CMS survey?
If deficiencies are found during the survey, we help you create a Plan of Correction (POC) and work with you until your agency meets all requirements. Our goal is to minimize delays and support you through every step until approval.
How do I know if my agency is eligible for Medicare or Medicaid certification?
Eligibility depends on your agency type (e.g., Home Health, Hospice, Assisted Living, Behavioral Health) and meeting federal and state licensing requirements. We’ll review your agency’s setup and guide you through the eligibility process before filing.
Will CarePolicy.US complete the forms for me, or just guide me?
We do both. Our team helps you complete and file all forms accurately and also provides consultation so you understand each step of the process.
Ready to Get Certified?
Starting your Medicare and Medicaid certification journey with us means partnering with experts who understand the full process from PECOS enrollment to survey readiness and state Medicaid approval. Contact us today to schedule your free initial consultation and take the first step towards expanding your services, reaching more clients, and securing timely reimbursements.


